Cancer is not a communicable disease—it doesn’t spread from person to person like infections caused by bacteria or viruses. Instead, cancer develops when certain cells in the body begin to grow uncontrollably due to genetic mutations or external risk factors such as smoking, radiation, or certain viruses. While some viruses (like HPV or hepatitis B and C) can increase the risk of developing specific cancers, the cancer itself remains non-contagious. Understanding this difference helps reduce fear, combat stigma, and supports a compassionate approach to cancer care and prevention.
What Is a Communicable Disease?
A communicable disease is an illness that can spread from one person to another through direct contact, shared air, contaminated food or water, or even insect bites. These diseases are caused by infectious agents like bacteria, viruses, fungi, or parasites. Common examples include flu, tuberculosis, and chickenpox. What makes them communicable is the fact that they can move between people or from animals to humans, unlike conditions such as cancer, which start inside the body and cannot be passed on through normal daily contact.
- Directly: through touch, coughing, sneezing, sexual contact, or mother to child
- Indirectly: via contaminated surfaces, food, water, or insect bites
Examples include tuberculosis, influenza, malaria, and COVID-19. These diseases are fundamentally different from cancer, which arises from internal cell changes rather than external infection.

Why Cancer Doesn’t Spread Like Infections?
Cancer develops because of changes or damage in a person’s own cells that cause them to grow and multiply uncontrollably. These changes are unique to each individual’s body and are not caused by germs like bacteria or viruses that can travel between people. Unlike infectious diseases, cancer doesn’t create agents that could leave one person’s body and infect another. Even if cancer cells were somehow transferred to another person, a healthy immune system would usually identify them as foreign and destroy them before they could grow.
- Cancer arises from internal cell mutations, not external infection.
- It cannot be transmitted through touching, hugging, or sharing meals.
- Cancer cells cannot survive and multiply in someone else’s body under normal circumstances.
Only in very rare cases, like certain organ transplants or from mother to baby, can cancer cells spread—and these are medical exceptions, not everyday risks.
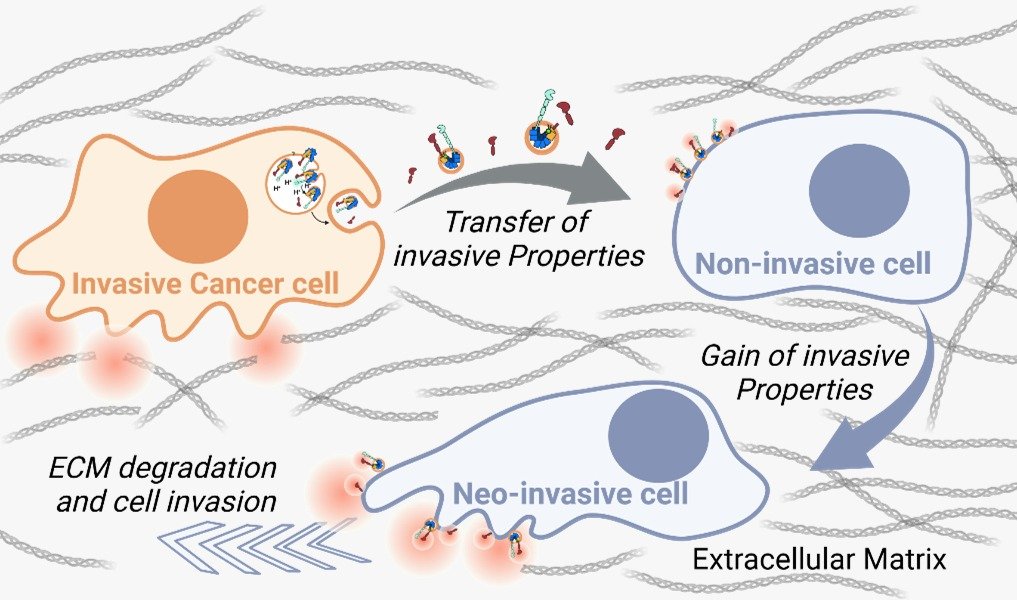
When Cancer Cells Can Be Transferred?
While cancer itself is not contagious in daily life, there are a few rare medical situations where cancer cells might pass from one person to another. These cases are extremely uncommon and usually involve special medical circumstances rather than normal social contact.
Some rare scenarios include:
- Organ or tissue transplantation: If an organ from a donor has hidden cancer cells, and the recipient’s immune system is suppressed to prevent rejection, those cells might grow.
- From mother to baby: Very rarely, cancer cells can cross the placenta during pregnancy and reach the baby.
- Linked to viruses: Certain viruses (like HPV or hepatitis B and C) can spread from person to person and may increase cancer risk — but in these cases, it is the virus that is contagious, not the cancer itself.
These rare instances remind us that while cancer cells can be transferred under specific medical conditions, they do not spread through normal daily contact like infections do.
How Homeopathy Supports Cancer Patients
Homeopathy does not claim to cure cancer itself, but it can play an important complementary role alongside conventional treatment. By focusing on the individual as a whole—mind, body, and emotions—homeopathy helps patients manage the challenges they face during and after cancer therapy, aiming to improve their quality of life and emotional resilience.
Some ways homeopathy can help include:
- Reducing side effects of chemotherapy and radiation, such as nausea, fatigue, mouth sores, and skin irritation.
- Supporting emotional well-being by easing anxiety, fear, and sleep disturbances.
- Strengthening the body’s natural vitality and immune response, which may help patients feel stronger and more balanced during recovery.
- Encouraging a more personalized, patient-centered approach, where remedies are selected based on individual symptoms and experiences.
While homeopathy should never replace standard cancer treatments, it can be a gentle, supportive addition that focuses on the patient’s overall comfort and well-being.

The Role of Prevention and Early Detection
Since cancer isn’t contagious, protecting ourselves and those we love depends on understanding risk factors, living healthier, and catching warning signs early. Prevention and early detection together can significantly lower the chances of developing advanced cancer and improve treatment outcomes if cancer is found.
- Healthy lifestyle choices: Avoiding tobacco, limiting alcohol, eating a balanced diet rich in fruits and vegetables, and staying physically active.
- Vaccinations: Protecting against cancer-related viruses like HPV (linked to cervical and throat cancers) and hepatitis B (linked to liver cancer).
- Regular screenings: Such as Pap smears, mammograms, colonoscopies, or prostate exams, based on age and personal risk factors.
- Being aware of family history: Sharing this information with your doctor to guide personalized screening plans.
Conclusion
Cancer is not a communicable disease—it doesn’t spread through touch, sharing food, or daily contact. While rare medical exceptions exist, they don’t change this fundamental truth. Instead of fearing cancer patients, we should focus on prevention, early detection, and supportive care like homeopathy to help manage side effects and emotional stress. With the right information and compassion, we can replace fear with understanding and truly support those affected by cancer.